Groundbreaking research published today in Nature Genetics describes the largest study ever into the genetics of random “time of day” blood glucose levels. The study, which includes nearly half a million people of various backgrounds, describes new types of DNA that affect blood sugar levels measured “abnormally.” A team of researchers, led by Professor Inga Prokopenko at the University of Surrey on behalf of the Meta-Analysis of Glucose and Insulin-related Traits Consortium (MAGIC), analyzed data from 17 large studies, including the UK Biobank.
This research has shown that individual responses to drugs from the popular class of GLP-1R agonists, used to treat type 2 diabetes and obesity, may depend on DNA variants in the target gene, GLP1R.
Scientists have also revealed, for the first time, that type 2 diabetes can directly cause lung problems. In the largest genetic study examining how genes affect blood sugar levels and health outcomes, researchers concluded that lung dysfunction should now be considered a complication of type 2 diabetes.
A study combining genetic data and expression sheds light on the importance of the gastrointestinal tract, where the small intestine, ileum, and colon play an important role in regulating blood glucose levels, in addition to the well-established role of the pancreas.
This very important study, involving more than a hundred scientists from all over the world, gives us new information on the genetics of blood sugar levels and type 2 diabetes. Now, we can better prevent type 2 diabetes complications, including lung disease. We need to improve treatment strategies for people with this condition, by studying individual DNA variants in relation to GLP-1R agonist response.
Professor Inga Prokopenko, e-One Health professor and Head of Statistical Multi-Omics from the University of Surrey
Individual genetic background influences GLP-1R agonist susceptibility.
GLP-1R agonists are used to treat people with type 2 diabetes to improve their glycemic control, meaning their ability to maintain blood sugar levels within the normal range. In addition, GLP-1R agonists have been widely recognized for helping people with type 2 diabetes lose weight, which can improve their health and quality of life. Scientists have made functional representations and structures of different DNA codes in the GLP1R (GLP-1 receptor) gene. The authors point out that the effect of GLP-1 receptor activity and response to GLP-1R agonist drugs may vary from one person to another depending on the type of GLP1R DNA coding variant they carry.
In general, patients carrying specific DNA variants in the GLP1R gene may not benefit from GLP-1R agonist therapy. Researchers suggest that doctors should pay more for people prescribed these drugs. By better matching the drug with the individual’s unique way of doing things, the treatment can work better for them.
Type 2 diabetes causes reduced lung function.
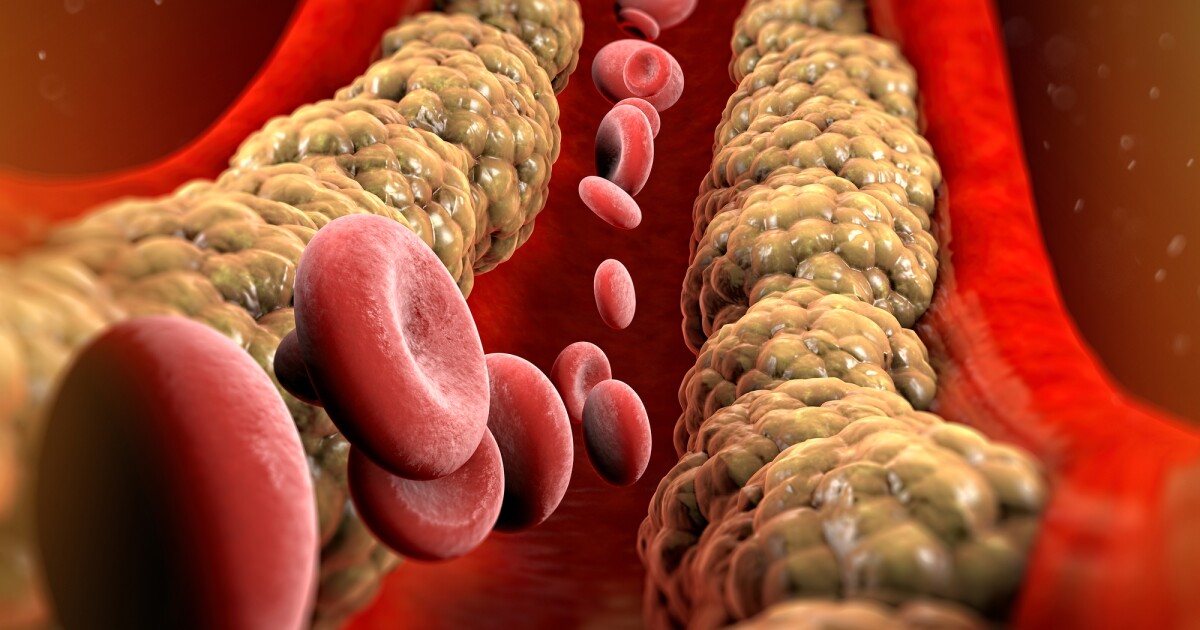
Previous studies have shown that lung conditions, including lung disease, fibrosis, and pneumonia, are more common in people with type 2 diabetes. However, until now, it was not known whether type 2 diabetes directly causes lung damage or whether other factors common to both conditions are responsible. To control for factors including smoking and sedentary behavior, the team used a statistical technique called Mendelian randomization to understand whether high blood sugar levels are linked to poor lung function and whether one causes the other. Lung function is measured using two standard spirometry tests. Analysis has shown that high blood sugar levels in people with type 2 diabetes directly affect lung function. For example, research data models have shown that an increase in blood sugar levels from 4 mmol/L to 12 mmol/L can cause a 20% decrease in lung function and function.
With respiratory disease the leading cause of death in England and hospital admissions for respiratory diseases in England and Wales doubling over the past 20 years, the findings highlight the need for health professionals to be vigilant about lung problems in people with type 2 diabetes. . Early detection and treatment of lung disorders can save the lives of thousands of people with type 2 diabetes.
The role of the gastrointestinal tract in the regulation of glucose levels.
The study identified the roles of tissues not previously implicated in glucose metabolism, particularly those in the gastrointestinal tract, especially the ileum and colon. It is known that the food eaten is received by the duodenum (the first part of the small intestine) and is mixed there with the digestive juice from the pancreas, liver and gallbladder. The jejunum and ileum also break down food and absorb nutrients from the blood.
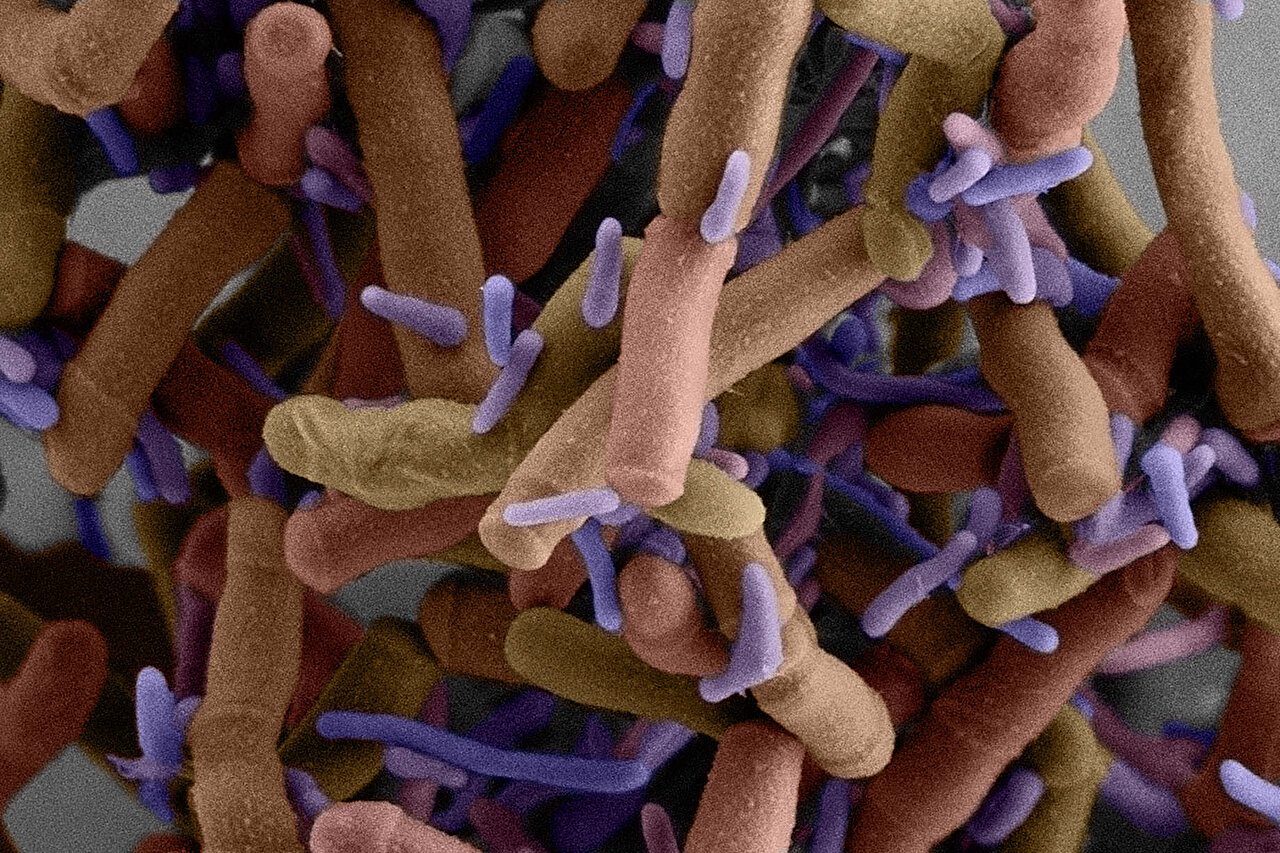
The large intestine, also called the colon, absorbs water and electrolytes from undigested food and hosts a diverse community of bacteria known as the gut microbiome. This study showed that the human gut microbiome and glycome are related to the regulation of glucose levels and emphasized the role of lactose- and galactose-based production of glucose by microbiomes Collinsella and Lachnospiraceae-FCS020.
Dr. Vasiliki Lagou, a postdoctoral scientist from the Department of Statistical Multiomics, first author of the paper, added:
“Our research provides the first evidence that high blood sugar levels in type 2 diabetes can directly lead to lung damage. We hope that our discovery that lung dysfunction is a complication of type 2 diabetes is the first step in increasing awareness among health professionals, which leads to the development of diabetes. early diagnosis and treatment of lung conditions.”
Dr Ayse Demirkan, Senior Lecturer in AI Multiomics for Health and Wellbeing at the University of Surrey, said:
“Our study sheds light on the less studied but highly influential role of the gastrointestinal tract in controlling blood sugar levels and type 2 diabetes. In addition to the pancreas, the small intestine and more specifically, the ileum and the colon, contribute to glucose metabolism, as characterized by gene expression in these tissues. In addition, we describe the relationship between the regulation of glucose levels and gut microbiome species, especially Collinsella and Lachnospiraceae-FCS020, which produce glucose from lactose and galactose.
Type 2 diabetes has many risk factors, including age, genetics, race and body weight.
Source:
Journal reference:
Lagou, V., continuous. (2023). Randomized glucose GWAS in 476,326 individuals provides insight into diabetes pathophysiology, complications and treatment stratification. Natural genetics. doi.org/10.1038/s41588-023-01462-3
#large #study #looked #genetics #clockwork #blood #sugar #levels